Stem cell transplant
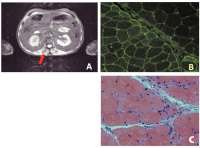
Figure 2a-c: A 36-year-old man received allogenic hematopoietic stem cell transplant
after non-Hodgkin lymphoma. Three months after the procedure, he developed
graft-versus-host disease (GVHD) with sicca syndrome and dermatitis. He was
treated with low-dose steroids and mycophenolate. Over the ensuing months,
mild proximal weakness and raised serum creatin-kinase appeared. He was
diagnosed with steroid myopathy by his haematologist and steroids were tapered.
On examination, he presented with scapular and pelvic weaknesses together
with severe cramps after voluntary contraction. EMG demonstrated myopathic
potentials and neuromyotonia. MRI showed a high STIR signal on axial muscles
(A, arrow) suggestive of muscle inflammation. A deltoid muscle biopsy was
performed. MHC type-1 expression of the muscle fibres in a perifascicular fashion
was demonstrated with immunofluorescence (B). Hematoxilin-eosin staining (C)
showed myopathic muscle fibres and inflammatory infiltrates. The patient was
diagnosed with myositis and neuromyotonia as a manifestation of GVHD. He was
treated with rituximab, mycophenolate, and low-dose steroids with gradual
improvement.
Keywords:
MRI,
non-Hodgkin lymphoma,
stem cell transplant